Rectal prolapse: All you need to know
Rectal prolapse is a common problem in the elderly with persistent constipation or weakened pelvic floor muscles. However, they are often confused with hemorrhoids because the early symptoms are quite similar. Therefore, we need to differentiate correctly to get the appropriate treatment. Let's come to the article to answer "all about rectal prolapse"!
content
- 1. What is rectal prolapse?
- 2. Who is susceptible to rectal prolapse?
- 3. What causes rectal prolapse?
- 4. What are the symptoms of rectal prolapse?
- 5. Is this another name for hemorrhoids?
- 6. How to diagnose?
- 7. Surgical treatment
- 8. How long will it take for me to recover from surgery?
- 9. Is rectal prolapse preventable?
1. What is rectal prolapse?
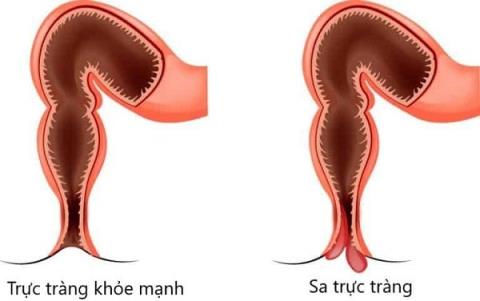
Rectal prolapse occurs when the lowest part of the large intestine (rectum) falls out of its normal position and slides out of the muscular opening at the end of the digestive tract (anus). This condition is divided into three types based on the movement of the rectum, namely:
- Intramural Rectal Prolapse : The rectum has begun to fall out of place but has not yet reached the anus.
- Partial rectal prolapse : Only part of the rectum has moved through the anus.
- Complete rectal prolapse : The entire rectum falls through the anus.
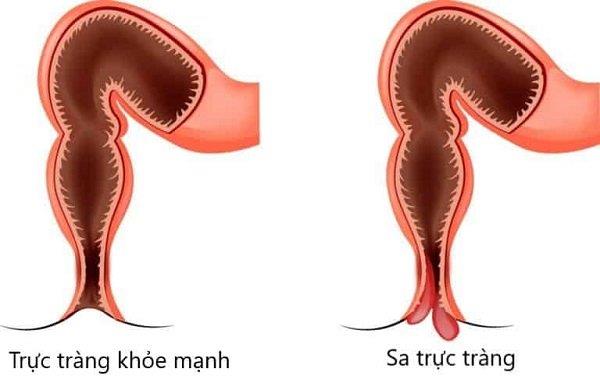
For some reason the rectum falls out of its normal position causing disease
2. Who is susceptible to rectal prolapse?
Rectal prolapse is more common in adults than children and more common in women than in men. The age of the disease is not the same for each sex. Most women develop rectal prolapse in their 50s or older, while most men develop it in their 40s or younger. In addition, in older women, rectal prolapse often occurs at the same time as uterine prolapse or bladder prolapse due to general weakness of the pelvic floor muscles.
3. What causes rectal prolapse?
Experts don't know for sure what causes rectal prolapse. However, several structural defects as well as risk factors have been identified that may increase this risk.
Structural Defects
In adults, a number of pelvic defects have been found such as:
- The rectum is more mobile than usual.
- Weakness in the pelvic floor and/or anal sphincter muscles.
In children, doctors found differences in the structure of the rectum. For example, the rectum does not bend as it should but stays in an upright position, increasing the risk of prolapse.
Risk factor
Any condition that increases pressure inside the abdomen or weakens the pelvic floor muscles can increase your risk. Examples include:
- Constipation or frequent diarrhea.
- Many births.
- Pelvic surgery
- Back injury or surgery/spinal cord injury.
- Intestinal parasitic infection
- Diabetes, Chronic Obstructive Pulmonary Disease (COPD),...
4. What are the symptoms of rectal prolapse?
Symptoms often vary as the disease progresses, often including:
- A red mass prolapsed outside the anus. At first, it may only happen during or after a bowel movement and is a temporary condition. However, over time – the rectum can prolapse with just standing or walking normally and it may be necessary to use your hands to push back up the anus.
- Pain in the anus and rectum.

The disease can cause burning pain in the anus and bloody stools
- Bleeding from the inner lining of the rectum.
- Incontinence (leakage of mucus, blood, or stool from the anus).
If you have any symptoms, you should see your doctor to get early treatment and prevent complications!
When these conditions persist, they can cause complications such as:
- Rectal ulcers cause heavy bleeding.
- Rectal prolapse (rectal prolapse cannot be pushed into the anus by hand). This is an emergency because the trapped intestine can lack blood supply leading to gangrene. You need to quickly go to the nearest medical facility for timely examination and treatment, to prevent sepsis, organ failure, shock, etc.
- Injury to the sphincter and nerves , leading to or worsening bowel incontinence.
5. Is this another name for hemorrhoids?
The answer is NO .
While hemorrhoids can also cause itching, anal pain, discomfort, and bleeding during bowel movements, they are essentially swollen blood vessels in the anal and rectal area. Meanwhile, rectal prolapse is the sliding of the contents of the terminal large intestine. However, in the early stages, rectal prolapse can look like an internal hemorrhoid that has slipped out of the anus, making it difficult to differentiate.
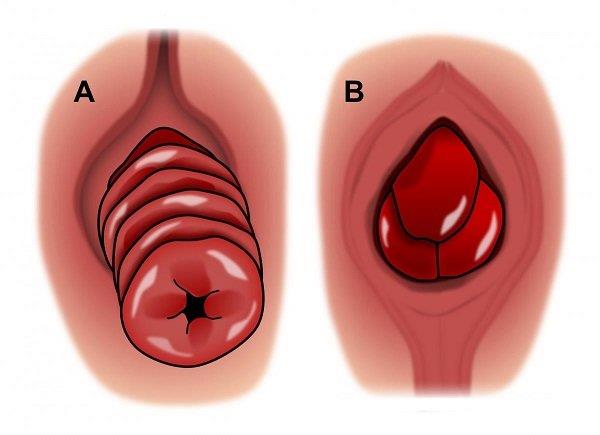
A: Rectal prolapse B: Hemorrhoids
If you suspect you have hemorrhoids or rectal prolapse, see your doctor for the best diagnosis and treatment!
6. How to diagnose?
First, your doctor will carefully review your symptoms and risk factors. Then, they perform an examination with measures such as:
- Direct observation of the anorectal area . Assess externally visible lesions.
- Rectal examination . The doctor will insert a gloved finger and lubricated with gel into the rectum to check for hidden lesions inside. Although they can be a little uncomfortable and confusing for the patient at first, they are very important to get an accurate diagnosis.
Several tests may be required to clarify the diagnosis or rule out other conditions, including:
- Proctography . Uses X-rays to create a video recording of the activity of the rectum. They are used to assess function and show structural changes in the rectum and anus.
- Colonoscopy/colonoscopy. The endoscope is inserted into the lumen of the intestine for a closer look at lesions that are not visible on examination. At the same time, the endoscope can also help the doctor perform a biopsy when needed.
- Endoscopic ultrasound. This test helps evaluate the shape and structure of the anal sphincter and surrounding tissues
- Additional tests. Used to check how well the nerves and muscles of the rectum and anus are working, such as an anal tonic.
7. Surgical treatment
In some very minor cases, treatment can start at home. However, surgery is often needed in the treatment of rectal prolapse.
In general, the two most common routes of access are abdominal and rectal. Within each approach there are different surgical methods that can be used to reposition the rectum. How to choose depends on many factors, including:
- Patient's age
- Degree of rectal prolapse
- Results of examinations and tests
- Other existing health problems
- The surgeon's preference and experience with certain techniques.
Abdominal surgery
- Commonly used in healthy young adults.
- In this approach, the patient is first given general anesthesia.
- Then, the doctor will make an incision in the abdomen and perform manipulations starting from this area.
Transrectal surgery
- Commonly used in elderly patients and in patients with multiple health problems.
- In this method, spinal or epidural anesthesia can be used instead of general anesthesia.
8. How long will it take for me to recover from surgery?
Most people make a full recovery from treatment for rectal prolapse and lead a normal life.
The average hospital stay is about 2 to 3 days and varies from patient to patient. Full recovery can take up to a month. However, to reduce the risk of recurrence, patients should limit strenuous exercise for at least 6 months, as well as have a healthy diet to prevent constipation. Such as:
- Eat a lot of fiber.
- Use dietary fiber supplements.
- Drink enough water.
- Use stool softeners (if necessary)
Note: Consult your doctor before taking any of the above medications and supplements to make sure they are right for you!
9. Is rectal prolapse preventable?
There are several lifestyle changes people can make to reduce their risk of rectal prolapse, such as:
- Eat lots of fiber.
- Drink a lot of water.
- Exercise regularly.
- Avoid pushing too hard during bowel movements.

Rectal prolapse is not a very serious condition. Treatment can be started at home, however, surgery is often needed. The hospital stay takes an average of 2 to 3 days and full recovery takes about a month. However, patients should limit heavy exercise for at least 6 months afterwards to reduce the possibility of disease recurrence. Please share to let everyone know!
Doctor Nguyen Ho Thanh An