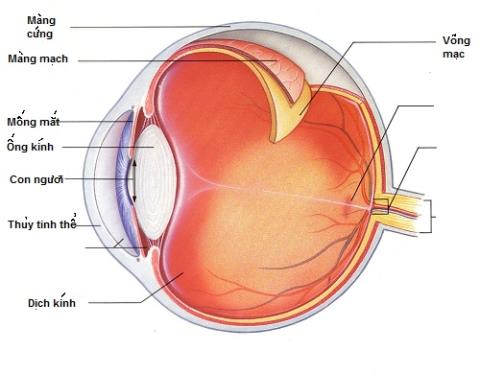
Gums are the lining of the mouth, directly related to the teeth. It covers the alveolar bone and surrounds the neck of the tooth. Through embryonic development, gums are also formed and acquire the shape when teeth erupt. Gums perform many important functions: adhesion, stability, bonding of teeth, creating a protective layer for bacteria. Here, let's learn about the composition, structure, function and characteristics of clinically healthy gum tissue with SignsSymptomsList.
content
1. Components of the gums
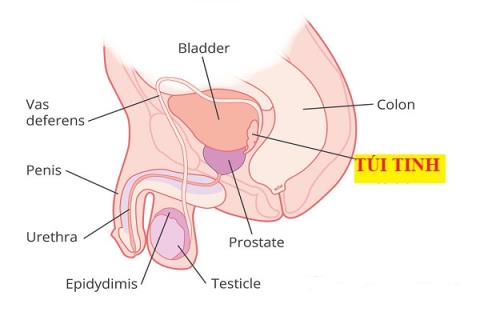
The gums are limited at the cervical side by the gingival margin. Apically by different parts of the oral mucosa:
- On the outside of the two jaws and on the inside of the mandible: the gingiva is continuous with the alveolar mucosa by the gingival-mucosal junction.
- On the palatal side: continuous gingiva with hard palatal mucosa.
Physically
Gums are divided into 2 zones:
- The outer and inner regions: gingival margins and gingival adhesions.
- Between teeth: Gums of papillae between teeth.
The gums of each region have 2 parts
- Free part: gingival margin.
- Adhesions: Adhesions.
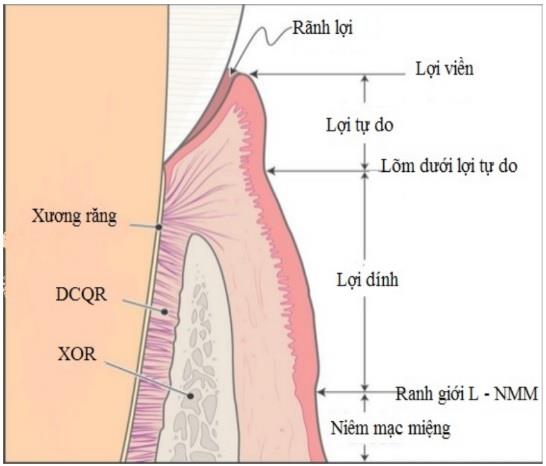
1.1. Edge gingiva (free gingiva / detached gingiva)
It is limited from the gingival margin (gingival margin) to the gingival sulcus. It is the part of the gum that surrounds the neck of the tooth. The gingiva does not adhere directly to the neck of the tooth and forms the soft wall of the gingival cleft. On a fully erupted tooth, the gum line covers the enamel. The gingival margin is about 0.5 - 2mm from the neck of the tooth and curves along the enamel-cement junction.
1.2. Sticky gums
Is the gingival part that limits from the gingival groove to the gingival-mucosal junction. In the absence of inflammation, sticky gums are clearly defined. Except in the palate there is no boundary between the sticky gingiva and the palatal mucosa. Adhesive gums have no loose connective tissue layer, less collagen fibers, more elastic fibers thicken, firmly adhere to the teeth and underlying bone.
The sticky gum surface when blow-dry appears orange-stained. This feature varies with age (more clearly in adults than in children), between individuals (some people don't) and different regions of the mouth (the outer surface is more prominent than the inner surface). This is a form of functional adaptive differentiation.
Orange-spotted gingival surfaces are a feature of healthy gums. A reduction or loss of orange blotchiness is a common manifestation of gum disease. This surface feature is associated with the expression and degree of keratinization of the epithelium. This gingival part is created to withstand chewing force, brushing force and other functional resources.
The height of the sticky gums varies from 1 to 9 mm and tends to increase with age. Adhesive gums have the greatest height in the incisors region. This height decreases gradually in the canines and posterior teeth. The area with the shortest gingival adhesion is the area of the first premolar. This is where the brake and muscle grips are usually located. The variation in gingival height by dentition was similar in both primary and permanent dentition.
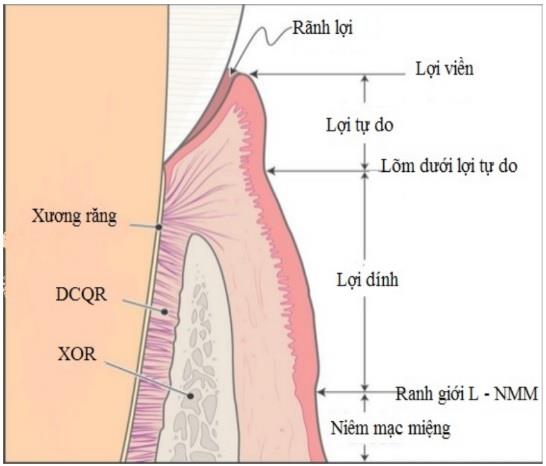
1.3. Groove gingival
A shallow concave line on the gingival surface that separates the free gingiva and the adherent gingiva. gingival sulcus (present only in 30-40% of adults). The position of the groove usually corresponds to the position of the base of the gingival fissure. The presence of gingival sulcus is independent of the state of the tooth with or without receding gums and the health of the gums.
See also: Have you properly cleaned your teeth?
1.4. Gum crevices
Is the limited space between the tooth and the free gingiva, whose base is the connecting epithelium. A clinically healthy gingival cleft usually does not exceed a depth of 3 mm. The gingival crevice depth measured with the pocket gauge may differ from the gingival cleft depth observed on the histological specimen.
1.5. Keratinized gums
Is the gingival band extending from the gingival margin to the gingival-mucosal junction. Thus, keratinized gingiva includes detached gingiva and adherent gingiva. The height of the keratinized gingiva varies from less than 1mm to 9mm.
Externally misaligned teeth such as canines and maxillary premolars often have a short superficial keratosis. The muscles and brakes attached low to the crown are often associated with a shortened gingival height.
In cases when there are no sticky gums, movement of the lips or cheeks causes tension on the gingival gingiva. This can increase the likelihood of receding gums. The appropriate gingival height level is the amount of keratinized tissue required to keep the gingival margin in a stable position and in a healthy state.
1.6. The gingival–mucosal junction
It is a scalloped curvilinear line that separates the keratinized gingiva and the alveolar mucosa. This line, especially on the outside, can be easily determined in three ways:
- Function: Use your hand to pull the lips or cheeks to see that the alveolar mucosa can be pulled up from the alveolar bone surface.
- Anatomy: The alveolar mucosa is darker red in color and the surface does not appear to be mottled with orange.
- Histochemistry of the alveolar mucosa was stained with Iodine Schiller solution.
See also: Gingivitis and periodontitis: What do you know?
1.7. Gum papillae (also called papillae)
Is the gum between adjacent teeth and fills the space between these teeth. Each space between two adjacent teeth, below the contact of these two teeth, has two gingival papillae: the outer gingival papilla and the medial gingival papilla. They are connected by a curved gingival saddle in the lateral-inward direction.
In the absence of contact between adjacent teeth, there are no gingival papillae and gingival saddle. Gums in this area are keratinized.
1.8. Gum recession between teeth
Are longitudinal grooves, parallel to the long axis of adjacent teeth, located between teeth in the gingival region.
2. Histological features
Gums are composed of epithelial, connective tissue, blood vessels, and nerves.
2.1. Gum epithelium
The gingival epithelium is a squamous squamous epithelium. From the gingival margin to the gingival junction, the mucosa is keratinized or parakeratinized, unlike the alveolar mucosa, which is non-keratinized. Keratinization is considered to be a process of differentiation rather than degeneration. The degree of keratinization of the oral mucosa varies by region and in descending order: from the palate, gums, sloth to cheeks. The degree of keratinization of the gums decreases with age and after menopause.
Gum epithelium can be divided into 3 types :
gingival epithelium
Is the epithelium of the gums in the oral cavity, covering the gingival surface and gingival adhesions. This epithelial part is completely uniform in thickness and nature.
gingival epithelium
Coating the gingival sulcus surface, similar in structure to the oral gingival epithelium. Except the surface cells may not be completely keratinized. It is less permeable than the connecting epithelium and is usually free of additional leukocytosis.
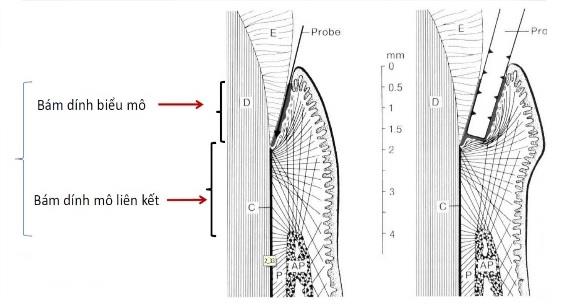
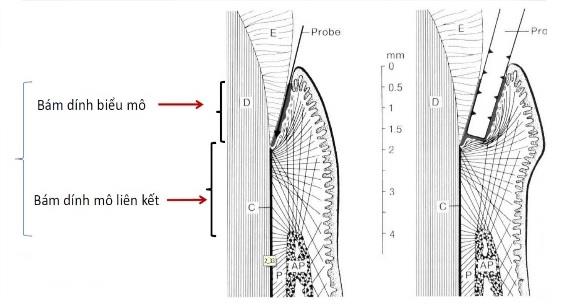
Connective epithelium (adhesion epithelium)
Continuous with the gingival epithelium, extending from the base of the gingival sulcus to the enamel-cementum junction (in case there is no gingival cleft, the epithelium connects from the gingival margin). This epithelium adheres to the tooth surface creating epithelial adhesions.
A distinctive histological feature of the connecting epithelium is the very high rate of cell turnover. Exfoliation from the base of the gingival crevice occurs 50 to 100 times more frequently than cell turnover at the gingival epithelial surface.
The position of the connecting epithelium on the tooth depends on the stage of eruption. In adults, this is at or near the meniscus seam. The apical migration from this position of the connective epithelium is considered to be a cephalopathy rather than a physiological process with age. The adhesion of this epithelium to the teeth is comparable to that of the epithelium and connective tissue in the skin or other surfaces in the body. The length of the connecting epithelium usually does not exceed 2 – 3mm.
2.2. Connective tissues
Similar to other tissues in the body, gingival connective tissue consists of: cells, fibers, matrix, and nervous vascular system.
Cell
Fibroblasts and fibroblasts make up the majority. Both of these cell types have high osteoblast-like phosphotase alcaline activity. Guard cells include:
- Nourishing cells.
- Myeloid cells: macrophages, monocytes, polymorphonuclear leukocytes
- Lymphocytes: T lymphocytes, B+ lymphocytes…
- Homologous cells.
- Auxiliary cells: antigen-presenting cells, platelets, endothelial cells.
The number of cells decreases with the age of the individual and is located in areas of reduced function.
Yarns
Mainly collagen and elastin. Collagen fibers are clustered in bundles and oriented.
Consists of three main groups: gingival group, ring group, transverse wall group.
- Gum group : consists of three bundles radiating from the cementum on the alveolar crest to the marginal gingiva, the adherent gingiva and the periosteum on the outer surface of the alveolar bone.
- Ring group : forming a ring or semi-circle surrounding the teeth. Radiates from the gingival margin to the crest of the bone.
- Transverse : these fibers cross the gingival connective tissue between two teeth, attaching the cementum on the alveolar crest of one tooth to the cementum on the alveolar crest of the adjacent tooth. Some authors classify this group of fibers as the major fibers of the periodontal ligament rather than the gingival fibrous system.
The fibrous bundles of connective tissue contribute to the formation of connective adhesions that function to support the connective epithelium, keep the gingival adhesion stable around the teeth and around the alveolar bone, hold the teeth together, and to a certain extent lower than keeping the tooth in the alveolar bone.
Blood circulation in the gums
Derived from three sources:
- The supraperiosteal blood vessels are terminal branches of the reticular artery, the sympathetic artery, the biliary artery, the great palatal artery, the suborbital artery, and the superior posterior dental artery.
- Blood vessels of the periodontal ligament : network with several capillary branches in the gingival cleft.
- Arterioles: the guava bone artery comes from the mid-dental septum, forming a network with the blood vessels of the periodontal ligament, with capillaries in the gingival cleft, and with blood vessels penetrating the alveolar bone.
See also: How is the set of teeth structured and what role does it play?
Lymphatic circulation in the gums
Lymphatic drainage begins from the lymphatic vessels in the gingival connective tissue papillae into the extraperiosteal collection system and then into the regional lymph nodes, especially the submandibular group. In addition, the lymphatic vessels just below the epithelium connect to the vessels in the periodontal ligament. The lingual and inner gingivae of the lower incisors drain into the subchin lymph nodes. The maxillary medial gingiva leads to the deep cervical lymph nodes. The remaining gingival areas (maxillary lingual gingiva, lingual lingual gingivae of mandibular premolar and premolar) all drain into the submandibular ganglion.
Nerve distribution in the gums
- The gingival nerves are nerve fibers from the maxillary, palatal, oral, and lingual branches (nerves V2, V3) and to a lesser extent from fibers in the periodontal ligament. Most of the gingival nerve fibers are associated with the supraperiosteal vessels of the alveolar bone forming the deep plexus.
- Nerves in the gums control heat and touch sensations.
See more: Do braces really change the face?
For the above function:
The superior dental branches of the infraorbital nerve supply the gingival surfaces of the maxillary incisors, canines, and premolars. Remaining gums on the lateral surface of the upper molars are due to the posterior maxillary nerve. The great palatal nerve distributes to the palatal mucosa except in the area of incisor caries caused by the naso-palatal nerve.
For the lower function:
The sublingual branch of the reticular nerve supplies the mandibular medial facial gingiva. The sciatic nerve supplies the lingual gingiva of the lower incisors and premolars. Remaining gums on the outer surface of molars are controlled by the oral nerve.
3. Function of the gums
- Contributes to the adhesion and stability of the teeth in the alveolar process.
- Links the individual teeth on a jaw into a continuous arch.
- Continuity of the oral mucosa is maintained by the connective epithelium that surrounds the neck of each tooth and adheres to the tooth surface.
- Create a peripheral defense against bacterial invasion.
4. The ability of gum tissue to renew and repair
Gum tissue has the ability to regenerate rapidly thanks to the high renewal rate of epithelial and connective tissue components.
4.1. Conversion speed and gingival resiliency
- The turnover rate of the epithelium is the amount of time it takes for a whole cell turnover. This period is 5 to 7 days, which is faster than the replacement rate of the oral epithelium (6 to 12 days).
- Gum re-epithelialization is the process of re-epithelialization following a mechanical injury. During this process, sloughing (sloughing) of the resulting epithelium continues from the remainder of the basal epithelium. Re-epithelialization and restoration of the adherent epithelium progress from the apex to the gingival margin, similar to the closure of a zipper.
If the gingival margin, including all of the connective epithelium, is removed by gingivectomy, a completely new connective epithelium will emerge within two weeks from the daughter cells of the basal gingival epithelium. . After complete healing, the connective epithelium (together with the adherent epithelium) is formed in this way.
4.2. Renewal and regenerative capacity of the gingival connective tissue component
The connective component of gum tissue is also replaced at a very rapid rate – much faster than alveolar bone or skin. The density and velocity of collagen are a function of the degree of concentration of the fibroblasts and their activity. See more: How should children with teething fever be treated?
5. Protective mechanism of gum tissue
Peripheral gingival lesions can be quickly repaired thanks to the strong regenerative capacity of gum tissue. This possibility must be considered in relation to the protective actions of gingival tissue.
Gums are located in a position that acts as the body's peripheral defense system. Connective epithelium plays a major role in this function. It is permeable in both directions. Without the humoral and cellular defenses of the junctional epithelium, bacteria from the plaque can invade the connective tissue and cause infection.
In the presence of inflammation, gingival exudates containing immunoglobulins penetrate the junctional epithelium. Simultaneously, neutrophils are also continuously migrating across the connective epithelium.
Neutrophils often congregate in areas of the epithelium as they move across them. Lymphocytes and macrophages reside in the intercellular spaces near the basal cell layer. Lymphocytes are self-limited to the epithelium. They can recognize antigens in the epithelium. Like the lymphocytes of the amygdala or the stomach and small intestine. They then retreat into the connective tissue and initiate specific immune responses.
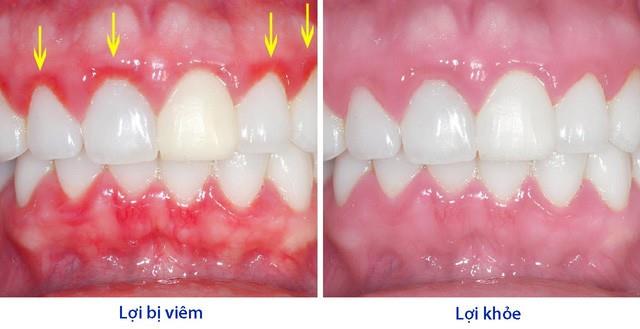
6. Clinical features of healthy gums
Normal healthy gums always show low-grade chronic inflammation. Due to the boundary between healthy gums and gingiva, pathological changes are quite vague.
True healthy gums are when there are no signs of inflammation when observing the histological specimen under the electron microscope. In these samples, the gingival epithelium was completely free of inflammatory cells. Connective tissue is devoid of white blood cells and extravascular blood cells.
The clinical presentation corresponding to this state is a qualitative criterion for healthy gums
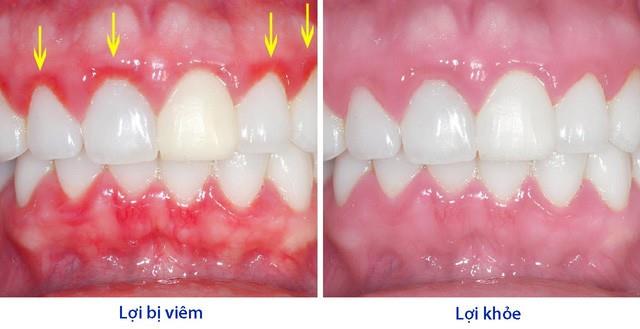
Healthy gums are usually pale pink. Compared with the more red color of the oral mucosa. Due to the thickness and keratinization of the gingival epithelial surface. The color of the gums in general can vary depending on: pigmentation, density, and blood flow through the tissue.
It looks orange when blow-dry, but the density of the spots varies considerably.
Depends on the shape and width of the interdental area. Or depends on the shape and position of the teeth on the dental arch.
+ Thin gum line, close to the teeth.
+ The gingival papillae is closest to the biting edge or chewing surface.
Healthy gums are firm, elastic, and cling tightly to the hard tissues underneath. The gingiva may be slightly movable and close to the tooth surface.
Depth varies from 1 to 3mm. No bleeding on proper examination. No gingival flow was detected.
Gums play an important role in the oral system. It not only covers, creates aesthetics for the mouth area. In addition, it also plays a protective role, preventing the invasion of bacteria. Understanding the structure and mechanism of protection and regeneration of gum tissue helps us to restore gums in cases of damage.
Doctor Truong My Linh